What exactly is CAR T-cell therapy?
What exactly is CAR T-cell therapy?
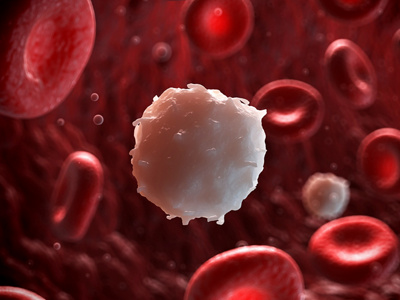
Blood can cure cancer: In CAR T-cell therapy, immune cells are genetically modified to recognise and fight cancer cells. The patient’s own immune cells are removed, processed in the laboratory and reintroduced via an infusion – no matching donor is needed.
Blood is made up of thousands of different cells. Some of these belong to a special group of white blood cells called T-cells. They are responsible for your body’s immune response system and find diseased or damaged cells, bind to them and destroy them. The problem for cancer patients is this: T-cells are practically blind to cancer cells and do not recognise them as a threat. However, with the help of genetic engineering, T-cells can be converted in the laboratory into Chimeric Antigen Receptor T-cells, or CAR T-cells for short. These synthetic T-cells can identify the diseased cells with their antigen-specific receptors. It is a breakthrough in cancer therapy.
What preparations are made before the treatment?
What preparations are made before the treatment?
Currently, CAR T-cell therapy is only intended for patients for whom all other treatment methods were unsuccessful. Patients need to have chemotherapy before the genetically modified cells taken from their bodies can be reintroduced. This prepares the body to absorb CAR T-cells so that they can work and replicate freely.
How is the treatment performed?
How is the treatment performed?
CAR T-cell therapy is based on autologous transplantation. This means that the cell donor is also the recipient. Blood is first taken from the patient’s veins and flows into a type of dialysis machine, where T-cells are filtered out in a blood purification process called leukapheresis, before the blood is returned to the body.
The cells obtained in this way are frozen and sent to specialist laboratories, where they are genetically engineered so the T-cells produce a protein that can recognise and bind to cancer cells. From this point on, they are called CAR T-cells. They are then replicated, tested and sent back to Klinik Hirslanden. This procedure takes up to 27 days.
Shortly before the CAR T-cells are transplanted, the patient receives chemotherapy. This destroys as many T-cells in the blood as possible, making it easier for the supplied CAR T-cells to spread. The cells processed in the laboratory flow into the bloodstream via an infusion. Their task is to replicate, detect and eliminate the cancer cells.
What is the success rate of the treatment?
What is the success rate of the treatment?
Most patients have been shown to respond very well to CAR T-cell therapy. However, what remains unclear is whether it is able to control the disease in the long term or even bring about a complete cure. Studies are currently being conducted with a view to introducing the therapy as early as possible during treatment and thereby obviating the need for other therapies.
What are the complications or risks of the treatment?
What are the complications or risks of the treatment?
Since CAR T-cell therapy involves blood being taken from the veins and reintroduced, the risk of infection and the physical strain on the patient during transplantation is low.
Chemotherapy weakens the immune system and after a CAR T-cell infusion, side effects can occur. These include inflammatory reactions, damage to the nerves, heart or blood vessels, or cytokine release syndrome (CRS), which can cause life-threatening fever, chills and breathing difficulties. As the treatment is still relatively new, the possible long-term effects have not been studied yet.
In addition, there is a residual risk that the cells will not be able to multiply in the laboratory or fight the tumour well enough in the body.
What happens after the treatment?
What happens after the treatment?
After the CAR T-cell transplant, patients stay in Klinik Hirslanden for between two and four weeks. This makes it possible to respond quickly if side effects occur and to observe the patient’s progress. Often the success or failure of the therapy can be decided as early as one to two months after the infusion. If the cancer cells can be eliminated, the patient then has regular check-ups with their attending doctor.
Centres 2
-
Tumour Centre Hirslanden Zurich
Witellikerstrasse 40 8032 Zürich
Please contact the attending physician directly to request the medical reports
Our oncology (consultation hours, appointments) can be reached at:
+41 44 387 37 80 or info@kho.ch
For questions/registrations for the Indikationsboards (for users) select:
+41 44 387 96 55 or indikationsboards@hirslanden.chFor administrative questions about quality certification, please contact us at:
+41 44 387 96 62


