A vertebral fracture, colloquially known as a fractured spine, is frequently caused by accidents, bone metastases from cancer or age-related bone weakness (osteoporosis). This injury affects the spine’s bony structures and can lead to severe pain and restricted movement. Modern surgical treatment for spinal fractures caused by osteoporosis consists of stabilisation and rebuilding the damaged vertebral body with bone cement. For spinal fractures caused by accidents, the fractured vertebrae are often treated with osteosynthesis procedures.
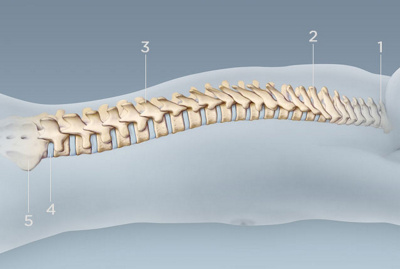
1. cervical vertebra (C1-7)
2. thoracic vertebra (Th1-12)
3. lumbar vertebra (L1-5)
4. intervertebral disc
5. sacrum
Spinal fractures at a glance
The spine consists of 24 movable vertebrae, which are flexibly connected by intervertebral discs to ensure stability and mobility. In the lower spine, several fused vertebrae merge to form the sacrum and the coccyx. A spinal fracture occurs when one of spine’s vertebral bodies is damaged or broken. These fractures usually manifest as a sudden onset of back pain, which can radiate into the buttocks, sides or chest.
Repeated fractures or a progressive spinal deformation can lead to visible changes such as a rounded back (‘dowager’s hump’) or a loss of height. If the fracture affects nerves or the spinal cord, symptoms such as a loss of sensation, paralysis or other neurological impairments may also occur.
Spinal fractures can be divided into two basic categories: pathological fractures caused by diseases such as osteoporosis or tumours, and traumatic fractures caused by an accident or fall.
Pathological spinal fractures
Starting from around the age of 40, humans gradually experience a decrease in bone substance. This process is called bone loss or osteoporosis and is the most common cause of vertebral fractures. Triggers for this include hormonal changes during menopause, which is why women are affected by osteoporosis much more frequently than men.
The bone loss in the vertebral bodies can lead to the vertebrae breaking even at low strain, for example when coughing or lifting heavy loads. This usually affects the thoracic or lumbar spine vertebrae, whereby the upper and lower surfaces of a vertebra – known as the base and top plates – collapse (fish vertebrae), or the leading edge of the vertebral body collapses, causing a spinal wedge. Such changes lead to spinal misalignments, which can be accompanied by deformities, limited mobility and back pain.
Traumatic vertebral fractures
A traumatic spinal fracture is usually caused by great force, such as in car accidents, falls from great heights or during sport activities. This can cause one or more vertebral bodies to become unstable or even collapse. In such cases, surgical stabilisation is usually necessary to prevent neurological symptoms and restore spinal stability.
Treatment goal
The primary objective of a spinal fracture surgery is to restore the spine’s the integrity and stability. The anatomically correct alignment of the vertebral bodies and stabilisation using suitable procedures should help to alleviate pain and improve the patient’s mobility.
Treatment procedure
Different spinal fracture treatment methods are used depending on the type of fracture and its severity. Which procedure is chosen is based on individual factors such as the patient’s age, their general state of health and the specific nature of the fracture.
Conservative treatment
Many age-related spinal fractures can be treated conservatively. In this case, it’s important to have good pain management with suitable medications and supportive measures such as physiotherapy and wearing stabilising spinal braces. As the spine cannot be completely immobilised, the symptoms can last for several weeks – sometimes up to three months. During the healing phase, regular X-ray monitoring is necessary to detect the fracture’s progress and potential misalignments in good time.
Kyphoplasty/vertebroplasty
Kyphoplasty and vertebroplasty are both minimally invasive procedures that are often used for osteoporotic fractures. For both procedures, only small incisions in the skin above the spinal fracture are necessary. During kyphoplasty, a balloon is inserted into the collapsed vertebral body and inflated to restore the original height. The resulting space is then filled with bone cement. In a vertebroplasty, bone cement is injected directly into the damaged vertebral body.
The fluid bone cement then spreads evenly throughout the damaged vertebra and hardens in a short time. This rebuilds and strengthens vertebra damaged by osteoporosis. A polymethyl methacrylate plastic is used as cement. In younger patients, a biodegradable form of cement is used, as younger bodies are usually able to rebuild bone substance on their own.
Open surgical stabilisation
Complex or unstable spinal fractures – resulting from a fall or accident, for example – often require open surgical stabilisation. This involves the use of osteosynthesis methods, in which screws and rods are implanted to permanently fixate the vertebral fracture and restore the spine’s natural axis. This procedure usually results in a partial stiffening of the affected spinal section and is known as spondylodesis or spinal fusion.
Preparation and precautions
Comprehensive diagnostic examinations, including an X-ray, computed tomography (CT) and magnetic resonance tomography are performed before the intervention to determine the nature and age of the vertebral fracture. In addition, standard preoperative tests such as blood tests, ECGs and blood pressure measurements are carried out to assess the patient’s general state of health.
Patients taking blood-thinning medications must discontinue these in good time before surgery in consultation with the attending doctor. It’s also important to fast for at least six hours before the intervention in order to minimise risks during anaesthesia.
Aftercare and recovery
After kyphoplasty/vertebroplasty
As the injected bone cement hardens quickly, the spine is usually able to support weight again on the same day. Patients can often get up shortly after the intervention and gently move around. A check-up is performed around four to six weeks after treatment to assess the healing process and identify potential complications at an early stage.
By strengthening and stabilising the vertebra, general complaints such as pain and restricted movement can be significantly improved. However, the bone loss itself, which is the root of all the problems associated with osteoporotic fractures, is not solved by the intervention. When it comes to osteoporotic spinal fractures, it’s therefore crucial to continue treating the underlying osteoporosis. This includes a holistic therapy plan that includes both targeted physiotherapy with movement and muscle strengthening exercises and medication for osteoporosis. The latter can slow down bone degradation and stabilise the bone structure.
After osteosynthesis
For cases of accident-related spinal fractures that were stabilised surgically with screws, rods or plates, the post-treatment proceeds in several phases. Immediately after the surgery, cautious mobilisation begins – under medical supervision – usually with the support of a physiotherapist.
Depending on the extent of the injury and the stability of the implants used, the strain on the spine may initially be limited. In many cases, wearing a support brace for several weeks is recommended. Regular follow-up checks, including imaging (e.g. X-ray or CT), take place in the first few weeks and months to check the position of the implants and the healing process.
Potential complications
Both vertebroplasty and kyphoplasty are well-established, low-risk routine procedures. Nevertheless, as with any surgical intervention, complications cannot be completely ruled out. On occasion, infections, bleeding, blood clots (thrombosis) or nerve damage can occur. In rare cases, small amounts of bone cement may migrate into surrounding tissue. This can cause local irritation or – if nerve structures are affected – neurological symptoms.
In open surgical interventions such as osteosynthesis, there is also a risk of fractures or implants loosening, particularly in the case of severely weakened bone tissue. Scarring, muscle pain or restricted movement in the area that was operated on can also occur.
Frequently asked questions
How dangerous is a spinal fracture?
The dangerousness of a vertebral fracture depends on its type and severity. While some fractures cause only minor discomfort and can be treated conservatively, others pose a significant risk – especially if the spinal cord or surrounding nerve structures are affected. In such cases, neurological impairments such as numbness, restricted movement or even paralysis can occur. This is why early diagnosis and targeted treatment are particularly important for avoiding permanent damage.
How long does it take for a spinal fracture to heal?
The healing time depends on the severity of the fracture, the treatment method selected and the patient’s general state of health. A complete recovery usually takes 6 to 12 weeks. More complex fractures or concomitant illnesses can take longer to heal.
Can a spinal fracture heal on its own?
A stable vertebral fracture, such as in the case of osteoporosis, can heal by itself with conservative treatment – provided the spine remains stable and no misalignment occurs. Regular X-ray monitoring is important to monitor progress.
Can a spinal fracture be operated on?
Yes. Unstable, deformed or painful spinal fractures are often treated surgically. The aim is to stabilise the spine, alleviate pain and minimise neurological risks.
What can be done for spinal fractures in old age?
For older people with osteoporosis-related spinal fractures, targeted osteoporosis treatment is essential in addition to treating the fracture itself. These include bone strengthening medications, calcium and vitamin D supplements and targeted physical therapy. In many cases, a minimally invasive intervention such as kyphoplasty can provide rapid pain relief.
Centres 8
-
Ortho Aarau
Schänisweg
CH-5001 Aarau -
Ortho Clinic Zurich
Monday to Friday
8.00 - 12.00
13.00 - 17.00